
Labor and delivery can be an intense time. You are trying to manage your pain while anticipating finally meeting your sweet new baby and making the best decisions to keep yourself and your baby healthy. When your provider suggests a second-stage intervention like a vacuum birth to help labor along and keep you and your baby safe, understanding the benefits and risks is a good idea.
A vacuum-assisted birth may also be called “vacuum extraction” or “operative vaginal birth,” though “operative vaginal birth” can also mean a forceps delivery. Understanding what a vacuum birth is, why it might be used, some benefits and risks, and recovery is essential.
What Is a Vacuum Birth?
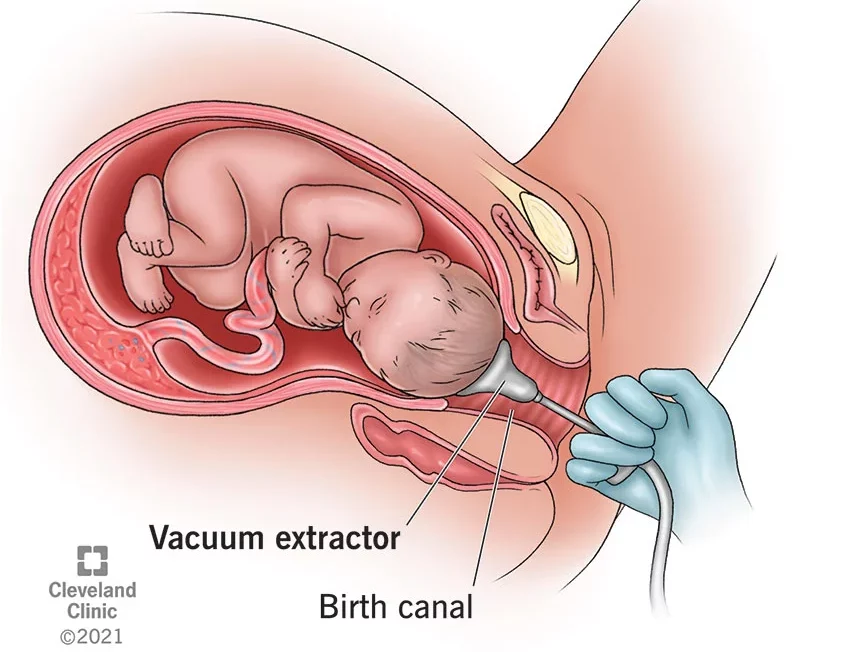
A vacuum birth uses a suction device to help quickly guide and pull the baby out of the birth canal. The suction device can be made of either metal or a softer material. The metal device is more likely to cause injury, but the soft material detaches from the baby’s head more often.1
A medical provider applies the vacuum to a specific spot on a baby’s scalp located over the hard area between the baby’s front and back fontanelles or soft spots. When correctly placed, the vacuum can help position the baby’s head to flex, rotate, and come down and out of the birth canal easily.1
Once a provider confirms the correct placement, they turn the suction on and increase it until the device indicates it is in the “green zone.” Your provider will pull down on the vacuum using one hand while using the other hand to make sure the device stays attached to the baby’s head. They apply suction each time you have a contraction and are pushing. The suction can stop once the baby’s head is visible and emerging, and the rest of the delivery proceeds normally.1
Why Might You Have a Vacuum Birth?
Vacuum birth can speed up a vaginal delivery if the mom or baby is not tolerating labor and the baby needs to come out quickly. It is faster than a C-section, which can be critical if the baby is in danger. It is also less invasive than a C-section, especially when the baby has already descended into the pelvis. This usually makes for an easier recovery for the mother.2,3
Some maternal indications for vacuum birth include exhaustion, a prolonged pushing phase, or pre-existing cardiovascular or neurological conditions preventing her from pushing.1
Your provider might also perform a vacuum birth if fetal heart rate issues indicate the baby is not tolerating contractions or pushing.1
When Can a Vacuum Birth be Done?
Pregnancy should be at least 34 weeks along for your provider to consider a vacuum delivery.1
Vacuum birth can only be used during the second stage of labor or the pushing phase. This means the cervix must be fully dilated, and the baby’s head must be engaged in the mother’s pelvis. Your bag of waters must also be broken.1
Other requirements for vacuum delivery include the following:1
- An empty bladder
- A pain control plan in place, such as an epidural
- An estimate that the baby’s head will fit through the mom’s pelvis
To start a vacuum birth, your provider must have your informed consent for the procedure and a backup plan for a C-section if the vacuum delivery fails.1
How Common is Vacuum Birth?
Vacuum birth accounts for 3-5 percent of all vaginal births in the United States. They are much more common in the South and less common in the Northeast.2,4
As the C-section rates have climbed, vacuum and forceps deliveries have decreased. You are only eligible for an attempted vacuum birth if you and your baby meet all the criteria.2
How Effective is Vacuum Birth?
Vacuum birth is very effective if used only on eligible patients and performed by experienced doctors. One study showed that an attempted vacuum extraction failed less than 5 percent of the time it was used. Vacuum births are more likely to fail in larger, older babies, taller mothers, experienced mothers, and moms with an epidural or Pitocin augmentation.4,5
If a vacuum-assisted delivery is unsuccessful within two or three pulls, or the device pops off the baby’s head more than three times, your provider should discontinue attempts and perform a C-section. A vacuum should not be applied for more than 20 to 30 minutes.1
Potential Risks of Vacuum Birth
Though the rates of serious complications associated with vacuum birth are relatively low, the mother and the baby can suffer consequences.
Maternal Complications
A mother may suffer from vaginal lacerations and vaginal and sphincter pain from a vacuum birth. Your provider should use a finger to ensure that no vaginal or cervical tissue is between the vacuum and the baby’s head before suctioning. This helps to decrease the risk of vaginal injury. Mothers may also experience painful urination, difficulty passing urine, or leakage of urine after a vacuum delivery.1,2
Fetal Complications
Vacuum birth poses certain risks to the baby from applying suction to their scalp. These risks include bruising and bleeding on the scalp, bleeding within the brain or eyes, high bilirubin levels, and neurological injury. Babies can also suffer skull fractures from vacuum delivery, which are typically minor and heal quickly. Rarely, a skull fracture might need surgery to repair.1,2
Alternatives to Vacuum Birth
If the risks of vacuum delivery are too high, you can continue laboring as normal. This is called expectant management. Expectant management may be more effective if you turn down having an epidural. This allows you to feel the urge to push and push more strongly. “Laboring down,” or waiting to push even after you are fully dilated, which allows your baby to descend independently, can also increase the success of expectant management.4
However, if there is a fetal emergency, your provider will likely advise some intervention instead of watchful waiting. If vacuum assistance is not the intervention of choice, it will either be Pitocin augmentation to strengthen and speed up your contractions and get the baby out or a Cesarean section.4
What is Recovery Like After a Vacuum Birth?
If there are no serious complications following a vacuum birth, your recovery will be like any other vaginal birth. Soreness and stinging are normal; your provider may recommend over-the-counter pain medication for relief. If soreness persists, pelvic floor physical therapy can help you fully recover.2
If you suffer from any vaginal tearing and receive any stitches, your stitches may burn or itch, especially during urination. These stitches usually dissolve independently, or your provider may remove them at your follow-up appointment at six weeks postpartum.
You will experience lochia, or postpartum vaginal bleeding, for the next six weeks while the uterus clears any remnants of pregnancy. This is usually normal and not related to having a vacuum-assisted birth. If the amount of blood you lose concerns you, contact your provider.2
Your baby should also recover from a vacuum birth over a few weeks. Any bruising, swelling, and jaundice should gradually disappear, or they may be put under blue lights to help jaundice levels come down. Be gentle with your baby’s fragile head during the first few weeks of life. Be sure to attend all pediatric appointments for your new baby to ensure they recover, heal, and grow as they should.2
Having an understanding in advance of potential labor and delivery interventions can help you to anticipate outcomes. During your prenatal appointments, you can ask your provider about their experience and comfort with vacuum birth if you need help during pushing. While it is not the first-choice delivery form, vacuum birth can help many women achieve a vaginal delivery quickly while keeping themselves and their babies safe.
Sources
1. https://www.ncbi.nlm.nih.gov/459234/
2. https://my.clevelandclinic.org/22305
3. https://utswmed.org/mbfvb
4. https://www.ncbi.nlm.nih.gov/2672989/
5. https://pubmed.ncbi.nlm.nih.gov/26967343/
from Baby Chick https://ift.tt/3VIbu8i
via IFTTT


0 Comments
Please ,
Don't enter span link ...